Phoebe, daughter of Bill Gates, suffered from Obsessive Compulsive Disorder (OCD) for many years.
https://www.gatesnotes.com/Books/Turtles-All-the-Way-Down?WT.mc_id=20180331120000_TurtlesAllTheWayDown_BG-FB&WT.tsrc=BGFB&linkId=49899518
Here’s what Phoebe had to say:
“For years I have been a loyal John Green fan—devouring his novels in the back of coffee shops, while traveling, and curled up on my couch. Something about the imagery of his books makes me get caught up in the fantasy of his stories, but Turtles All the Way Down hit closer to home for me than the rest. As someone who has struggled with OCD for years, I saw some of myself in the main character. But more than anything, this book struck close to home due to the intriguing character of Davis.
“Never has a book been able to capture so well what it is like to live in the shadow of someone else’s legacy. This story shows how Davis struggled to find his own identity outside of his father’s fame and wealth. Although we have very different relationships with our dads, I recognized his struggle, which also plays into my own life as I find my way in this world. This read was captivating like none other I have read before.”
https://www.gatesnotes.com/Books/Turtles-All-the-Way-Down?WT.mc_id=20180331120000_TurtlesAllTheWayDown_BG-FB&WT.tsrc=BGFB&linkId=49899518
Obsessive–compulsive disorder
| Obsessive–compulsive disorder | |
|---|---|
 | |
| Frequent, excessive hand washing occurs in some people with OCD | |
| Specialty | Psychiatry |
| Symptoms | Feel the need to check things repeatedly, perform certain routines repeatedly, have certain thoughts repeatedly[1] |
| Complications | Tics, anxiety disorder, suicide[2][3] |
| Usual onset | Before 35 years[1][2] |
| Causes | Unknown[1] |
| Risk factors | Child abuse, stress[2] |
| Diagnostic method | Based on the symptoms[2] |
| Similar conditions | Anxiety disorder, major depressive disorder, eating disorders, obsessive–compulsive personality disorder[2] |
| Treatment | Counseling, selective serotonin reuptake inhibitors, tricyclic antidepressants[4][5] |
| Frequency | 2.3%[6] |
Obsessive–compulsive disorder (OCD) is a mental disorder where people feel the need to check things repeatedly, perform certain routines repeatedly (called "rituals"), or have certain thoughts repeatedly (called "obsessions").[1] People are unable to control either the thoughts or the activities for more than a short period of time.[1] Common activities include hand washing, counting of things, and checking to see if a door is locked.[1] Some may have difficulty throwing things out.[1] These activities occur to such a degree that the person's daily life is negatively affected.[1] This often takes up more than an hour a day.[2] Most adults realize that the behaviors do not make sense.[1] The condition is associated with tics, anxiety disorder, and an increased risk of suicide.[2][3]
The cause is unknown.[1] There appear to be some genetic components with both identical twins more often affected than both non-identical twins.[2] Risk factors include a history of child abuse or other stress-inducing event.[2] Some cases have been documented to occur following infections.[2] The diagnosis is based on the symptoms and requires ruling out other drug related or medical causes.[2] Rating scales such as the Yale–Brown Obsessive Compulsive Scale (Y-BOCS) can be used to assess the severity.[7] Other disorders with similar symptoms include anxiety disorder, major depressive disorder, eating disorders, tic disorders, and obsessive–compulsive personality disorder.[2]
Treatment involves counselling, such as cognitive behavioral therapy (CBT), and sometimes medication, typically selective serotonin reuptake inhibitors (SSRIs).[4][5] CBT for OCD involves increasing exposure to what causes the problems while not allowing the repetitive behavior to occur.[4] While clomipramine appears to work as well as SSRIs, it has greater side effects.[4]Atypical antipsychotics may be useful when used in addition to an SSRI in treatment-resistant cases but are also associated with an increased risk of side effects.[5][8] Without treatment, the condition often lasts decades.[2]
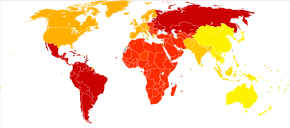
Obsessive–compulsive disorder affects about 2.3% of people at some point in their life.[6] Rates during a given year are about 1.2%, and it occurs worldwide.[2] It is unusual for symptoms to begin after the age of 35, and half of people develop problems before 20.[1][2] Males and females are affected about equally.[1] In English, the phrase obsessive–compulsive is often used in an informal manner unrelated to OCD to describe someone who is excessively meticulous, perfectionistic, absorbed, or otherwise fixated.[9]
Epidemiology
Obsessive–compulsive disorder affects about 2.3% of people at some point in their life.[6] Rates during a given year are about 1.2% and it occurs worldwide.[2] It is unusual for symptoms to begin after the age of thirty five and half of people develop problems before twenty.[1][2] Males and females are affected about equally.[1]
Associated conditions
People with OCD may be diagnosed with other conditions, as well as or instead of OCD, such as the aforementioned obsessive–compulsive personality disorder, major depressive disorder, bipolar disorder,[99] generalized anxiety disorder, anorexia nervosa, social anxiety disorder, bulimia nervosa, Tourette syndrome, Asperger syndrome, attention deficit hyperactivity disorder, dermatillomania (compulsive skin picking), body dysmorphic disorder and trichotillomania (hair pulling). More than 50 percent of people experience suicidal tendencies, and 15 percent have attempted suicide.[7] Depression, anxiety and prior suicide attempts increase the risk of future suicide attempts.[100]
Individuals with OCD have also been found to be affected by delayed sleep phase syndrome at a substantially higher rate than the general public.[101] Moreover, severe OCD symptoms are consistently associated with greater sleep disturbance. Reduced total sleep time and sleep efficiency have been observed in people with OCD, with delayed sleep onset and offset and an increased prevalence of delayed sleep phase disorder.[102]
Behaviorally, there is some research demonstrating a link between drug addiction and the disorder as well. For example, there is a higher risk of drug addiction among those with any anxiety disorder (possibly as a way of coping with the heightened levels of anxiety), but drug addiction among people with OCD may serve as a type of compulsive behavior and not just as a coping mechanism. Depression is also extremely prevalent among people with OCD. One explanation for the high depression rate among OCD populations was posited by Mineka, Watson and Clark (1998), who explained that people with OCD (or any other anxiety disorder) may feel depressed because of an "out of control" type of feeling.[103]
Someone exhibiting OCD signs does not necessarily have OCD. Behaviors that present as (or seem to be) obsessive or compulsive can also be found in a number of other conditions as well, including obsessive–compulsive personality disorder (OCPD), autism, disorders where perseveration is a possible feature (ADHD, PTSD, bodily disorders or habit problems)[104] or sub-clinically.
Some with OCD present with features typically associated with Tourette's syndrome, such as compulsions that may appear to resemble motor tics; this has been termed "tic-related OCD" or "Tourettic OCD".[105][106]
A myth propagated by Sigmund Freud regarding above-average intelligence in OCD was recently refuted.[107]
OCD frequently co-occurs with both bipolar disorder and major depressive disorder. Between 60%-80% of those with OCD experience a major depressive episode in their lifetime. Comorbidity rates have been reported at between 19%-90% due to methodological differences. Between 9%-35% of those with bipolar disorder also have OCD, compared to the 1%-2% in the general population. Around 50% of those with OCD experience cyclothymic traits or hypomanic episodes. OCD is also associated with anxiety disorders. Lifetime comorbidity for OCD has been reported at 22% for specific phobia, 18% for social anxiety disorder, 12% for panic disorder, and 30% for generalized anxiety disorder. The comorbidity rate for OCD and ADHD has been reported as high as 51%.[108]
Prognosis
Quality of life is reduced across all domains in OCD. While psychological or pharmacological treatment can lead to a reduction of OCD symptoms and an increase in QoL, symptoms may persist at moderate levels even following adequate treatment courses, and completely symptom-free periods are uncommon.[109][110] In pediatric OCD, around 40% still have the disorder in adulthood, and around 40% qualify for remission.[111]
No comments:
Post a Comment