HEALTH
Food Science Is Caught Between the Head and the Heart
"Heart-healthy" foods could be bad for the brain, new research suggests. What's a careful eater to do?
By
3
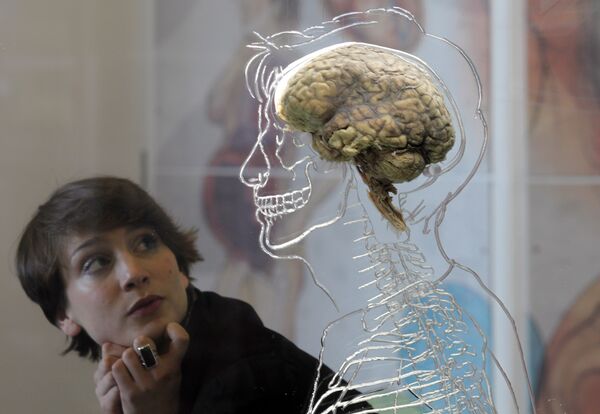
Isn't it beautiful?
Photographer: Matt Cardy/Getty Images
A few weeks ago, a scientific claim linking canola oil to Alzheimer’s disease risk raised an intriguing question: When it comes to healthy eating, do we have to choose between the head and the heart? In other words, is it possible that foods promoted as good for cardiovascular health, such as canola oil, are bad for the brain?
There’s surprisingly little information out there on what to eat for brain health. The vast majority of nutrition research is aimed at the heart. Why wouldn’t scientists want to focus on maintaining the seat of consciousness, memory, creativity, love, learning and joy, as opposed to a glorified pump?
Sure, hearth disease is the leading cause of death in the United States. But disorders of the brain may cause more suffering, and the numbers are growing. According to a new report, more than 6 million Americans currently live with Alzheimer’s disease, and by 2060, that will rise to 15 million. Given the choice, I’d much rather live with a faltering heart and a mint-condition brain than the other way around.
Since many of us are starved for information on brain health, it’s not surprising that news outlets played up the scare factor on the canola oil study, even though the deleterious effect was found in mice and therefore may not apply to humans.
The researchers, from Temple University in Philadelphia, conducted two studies, the first using olive oil and the second, canola, which is found in many processed and pre-prepared foods. They used special mice with a genetic predisposition to develop Alzheimer’s disease, and gave one group a few drops of olive oil each day. The mice given olive oil did slightly better on memory tests, and, upon dissection, had fewer plaques in their brains than did those fed a standard mouse diet.
When they tried the same experiment with canola oil, they found the mice getting the extra oil did worse on memory tests and had built up more brain plaques. The results may not be sufficient to make anyone give up canola oil, but they do make an important point -- food affects the brain.
Some media critics, such as Mary Chris Jaklevic at Health News Review, chastised reporters for not putting this single study into context. But what context? Not that many scientists specialize in diet and the brain, and when I sought them out, people kept pointing me back toward someone I’d interviewed in 2011 -- Joseph Hibbeln, a biochemist and psychiatrist working at the National Institutes of Health.
His research has focused on a potential positive influence of one kind of fat -- omega-3 fatty acids, which are found in seafood and some plants. He’s led studies that suggested a connection between low intake of omega-3s and a host of ills, such as suicide, violenceand obesity. Drew Ramsey, a clinical psychiatrist specializing on nutrition, also notes that some controlled clinical trials have suggested omega-3 fatty acids improve symptoms of depression.
That’s the uncontroversial part, since omega-3 fatty acids are approved by the American Heart Association as part of the family known as polyunsaturated fats. Where it gets tricky is in the biochemistry, because, as Hibbeln explains, there’s a chemical competition between omega-3s and another kind of allegedly heart-healthy polyunsaturated fat: omega-6, which is found in cottonseed, sunflower, safflower and corn oils, as well as corn- and soy-fed factory-farmed poultry. (Canola and olive oil are in a different category called monounsaturated fats.)
The problem with omega-6 fatty acids, Hibbeln says, is that the more you eat, the lower the level of omega-3 fats in your bloodstream given the same omega-3 intake. This happens because both kinds of fat compete for an enzyme that converts them to a form the body can use. So if you care about eating to keep your brain healthy, evidence would suggest keeping your omega-3 levels high, and that would mean not foiling your effort by ingesting omega-6 fats.
The ratio of omega-6 fats to omega-3s has changed drastically over the last 75 years, as omega-6 fats went from about 1 percent to 10 percent of the human diet, and blood levels of omega-3 have plummeted. In the story I wrote in 2011 about Hibbeln’s work, he called it “the greatest dietary transformation in the history of Homo sapiens."
Whether omega-6 fats are heart-healthy depends on who you talk to. The American Heart Association’s recommendations continue to promote all polyunsaturated fats as healthy, and to demonize saturated fats -- the kind found in butter and other full-fat dairy products. There was one very large, controlled clinical trial comparing the effects of a typical diet to one in which most of the saturated fat was switched out for omega-6 rich corn oil. A re-analysis published last year concluded that people getting the corn oil had lower cholesterol numbers but were more likely to die.
Saturated fat is neutral in the tug of war between the omega-6 and omega-3 fats. There’s a body of studies suggesting that saturated fats are bad for the heart -- but much of this was done in rabbits. The human studies -- both observational and clinical -- have recently been called into question and continue to generate controversy.
What’s a health-conscious person to eat when the science is in such a state of disarray? The only fats that seem to be uncontroversial are omega-3 fats and olive oil. Canola oil is chemically similar to olive oil, but these new studies suggest they’re not interchangeable. As Hibbeln told me, the brain makes up 2 percent of the body by weight and uses up 25 percent of the energy we consume. Focusing more research on how to feed it seems like a no-brainer.
This column does not necessarily reflect the opinion of the editorial board or Bloomberg LP and its owners.
